Managing Pain at the End of Life
During palliative care, a person’s symptoms and medication needs can change quickly. Being prepared for these changes helps keep the person comfortable and improves their quality of life.
- Not recognising when a person is in pain, including breakthrough pain.
- Not noticing or responding to non-verbal signs of pain.
- Not giving pain medication due to staff concerns about addiction, speeding up death, or legal issues.
- Train and support staff to recognise signs of pain and manage it well in palliative care.
- Encourage open discussions within the care team.
- Reassure staff that providing pain relief is necessary, expected, and good clinical practice. It is also legal when used to ease pain and suffering.
- Set clear pain management procedures, including when to reassess pain and when to use extra medication for breakthrough pain.
- Make sure pain relief medicines are prescribed, given, and available 24/7.
- Reflect on your own views about death, dying, and pain relief.
- Check that staff can recognise non-verbal signs of pain.
- Review medications to understand how they are prescribed and given.
- Ask the person for feedback, or with their consent, ask their family, friends, or support network. If they cannot give consent, ask their substitute decision-maker.
- Make sure the person or their substitute decision-maker has a way to communicate their pain and how strong it is.
Effective pain management is critical
Relieving pain is a key goal in palliative care. Reducing suffering and ensuring comfort is a priority. Pain relief medicines must be prescribed, given, and available 24/7.
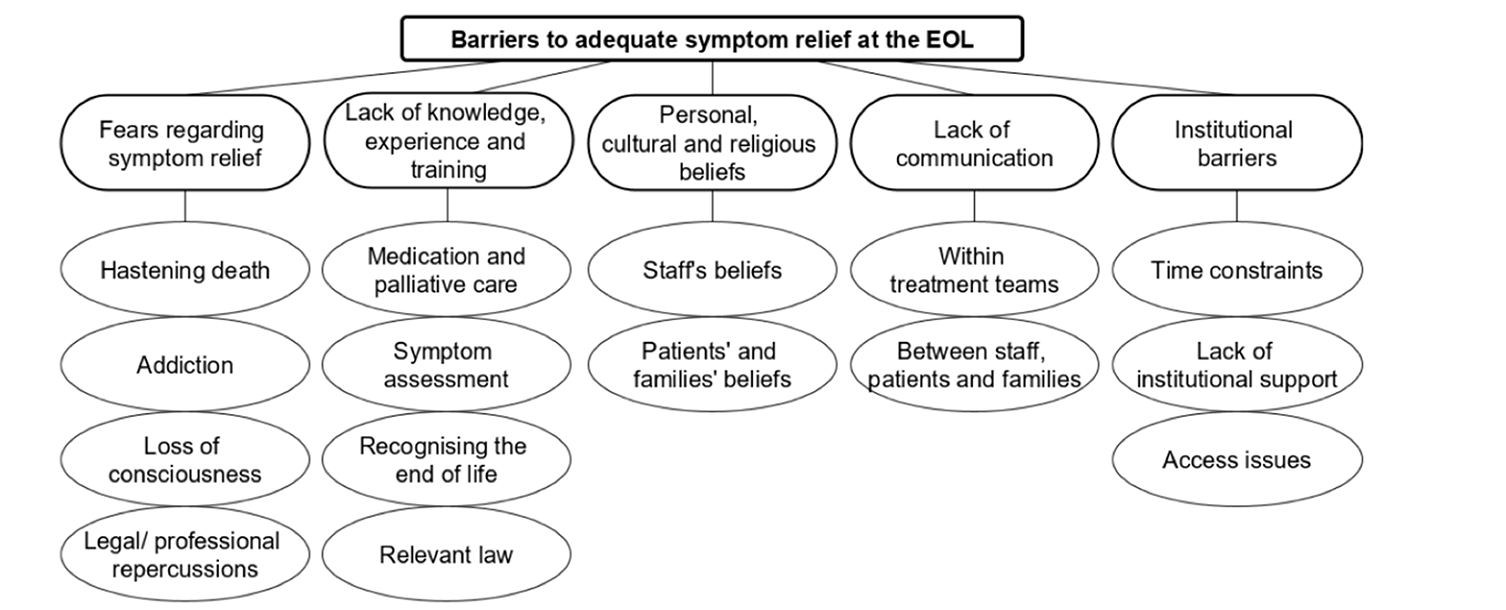
The diagram below shows barriers to pain relief found in a 2022 Australian study of nurses in end-of-life care, including aged care.
Staff must be aware of signs that a person is in pain, including breakthrough pain, which can occur between regular medication doses. It’s important to recognise how each person expresses pain, including non-verbal signs like grimacing, moaning, jaw-tightening, flinching, or clenching fists or blankets.
Good pain management requires staff knowledge and a supportive workplace. Open discussions can address concerns about giving pain relief and help dispel myths. Strong leadership support gives staff confidence in administering pain medication.
Concerns about addiction to high-dose pain relief, like opioids, should not prevent its use in palliative care when needed for comfort.
Some staff may worry that pain relief could hasten death or have legal consequences. In Australia, providing pain relief is legal when the goal is to ease pain and suffering, not to cause death.
Aged care providers and staff should recognise these challenges and work with the person, their family, and friends to find solutions.